Your Guide to Understanding the IVF Funnel and Success Rates

Medically reviewed by Linda Streety, RN, BSN
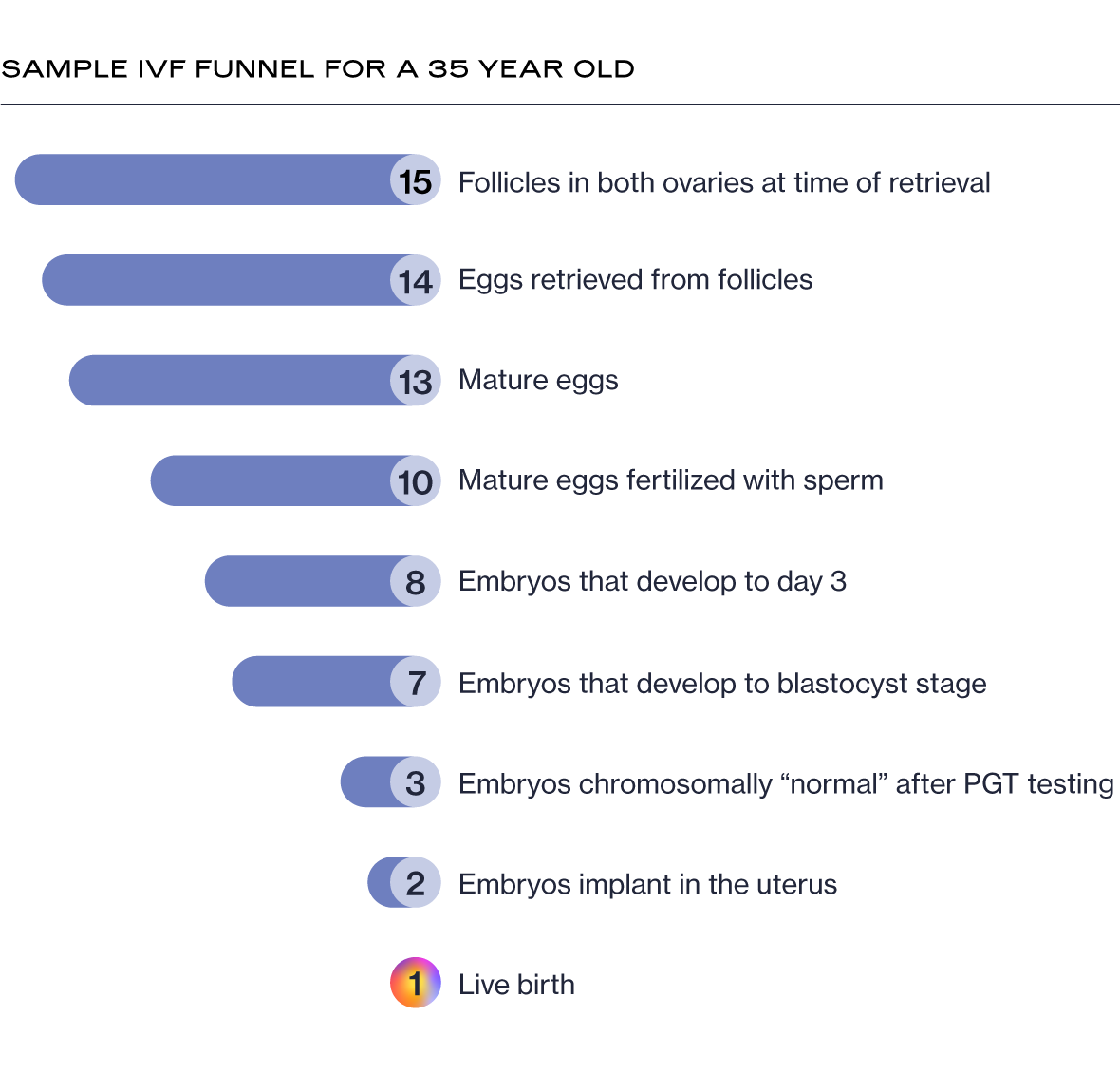
One of the most difficult parts of in vitro fertilization (IVF) is managing expectations and maintaining hope throughout the process. This can be challenging as you experience what we’ll refer to as the IVF “funnel.”
6 Second Snapshot
Since IVF treatment involves a complex series of procedures with delicate cells, some eggs and embryos don’t make it to the next step at each stage of the process.
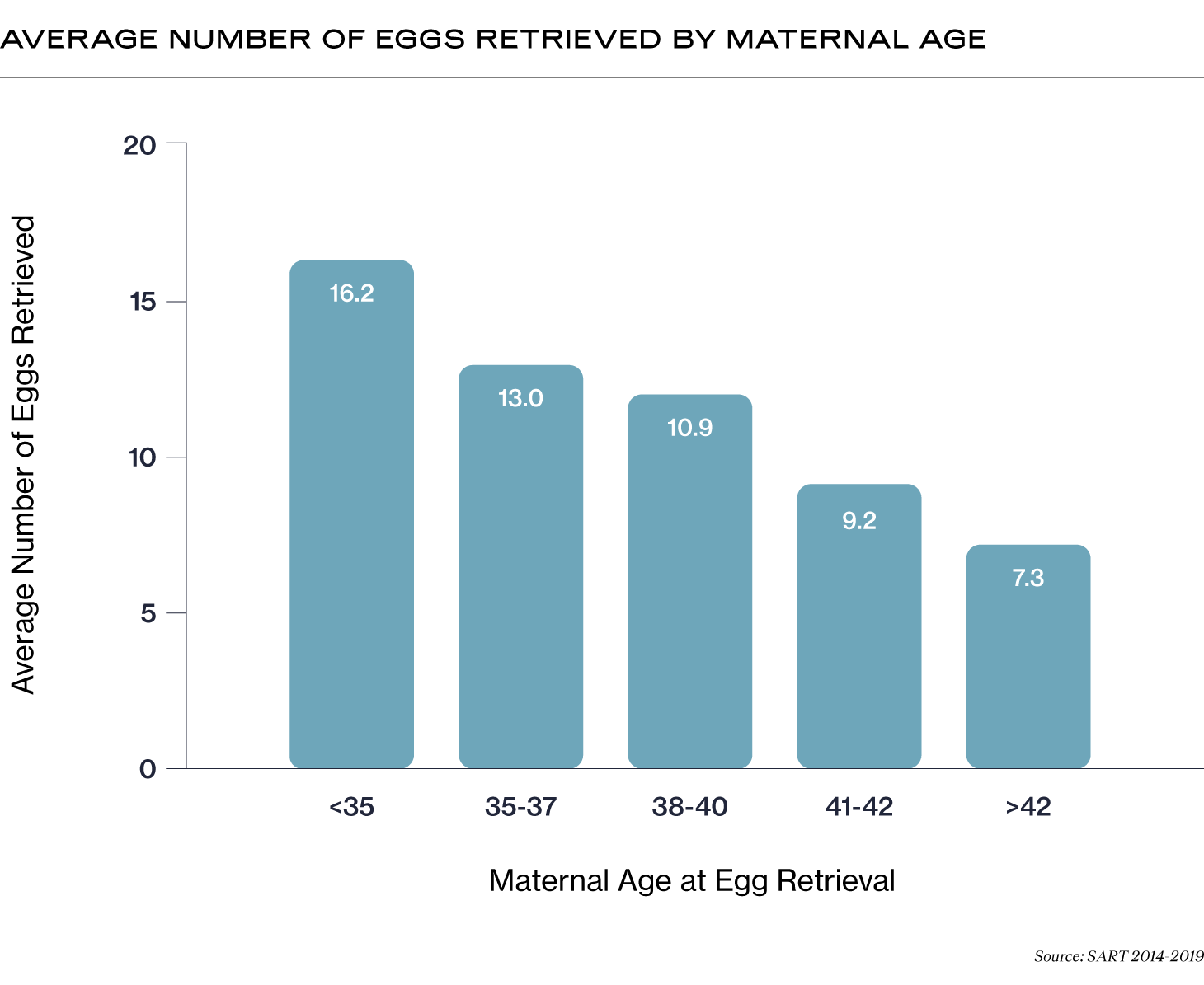
IVF success rates tend to vary by the age of the person with ovaries when the eggs were retrieved.
New research shows that safely retrieving more eggs gives you a greater overall chance of success
Number of Eggs Retrieved ≠ Number of Babies
To start, many patients believe that if 10 eggs are retrieved, they will end up with 10 embryos. However, since IVF treatment involves a complex series of procedures with delicate cells, some eggs and embryos don’t make it to the next step at each stage of the process.

Though it can feel disappointing if you aren’t prepared for it, this attrition is completely normal and expected. In fact, it’s possible to have many follicles (small, fluid-filled sacs in the ovaries in which eggs grow) but far fewer mature eggs after egg retrieval, or a handful of embryos after fertilization and only a couple that reach the blastocyst stage (when the embryo develops into two types of cells, the cells that will form the fetus and the cells that will form the placenta). Knowing what to expect throughout the process can help you maintain realistic expectations as you undergo IVF.
IVF Success Rates by Age
IVF success rates tend to vary by the age of the person with ovaries when the eggs were retrieved. Below is a graph showing the average live birth rate per IVF cycle (IVF cycle = when all the embryos created from an egg retrieval have been transferred to the uterus), according to the 2019 SART National Summary Report:
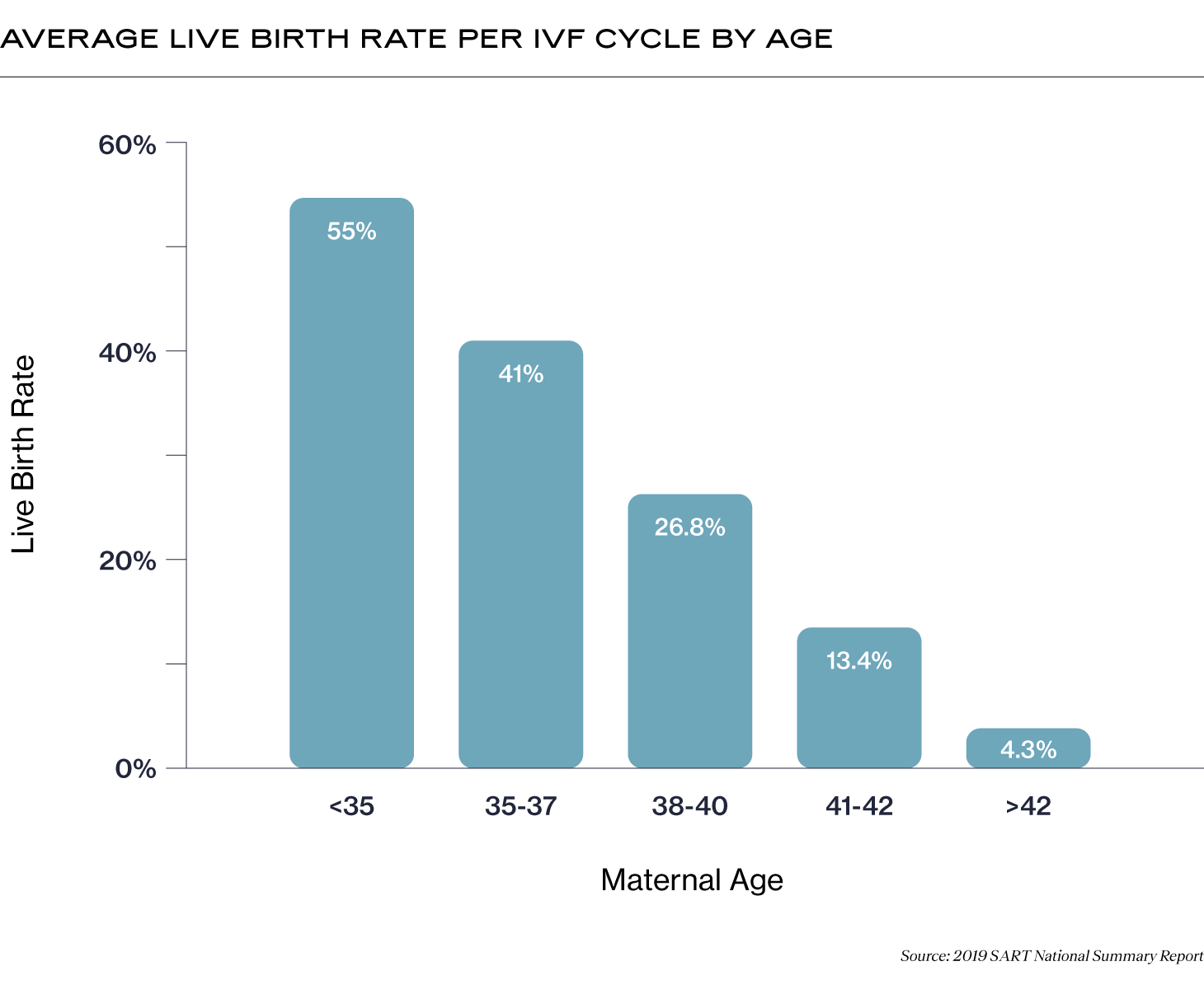
A lot of factors go into those numbers. Let’s go through the IVF process and explore how the IVF “funnel” might affect your results at each step.
Eggs Retrieved and Checked for Maturity
IVF begins with ovarian stimulation. Your reproductive endocrinologist (RE) will prescribe medications to stimulate your ovaries to produce more follicles than usual. After self-administering these medications for ~7-10 days and having your progress monitored closely by your fertility care team, your RE will schedule the egg retrieval procedure. During this procedure, a thin needle is guided through the wall of your vagina to withdraw fluid from each of your follicles. Within that fluid will be your eggs!
It’s very common that the number of eggs retrieved will be fewer than the number of follicles your RE counted on the ultrasound screen during ovarian stimulation.
In general, there’s a decrease in the average number of eggs retrieved by age (1).
The rule of thumb used to be that 15 eggs was the optimal number of eggs to retrieve per cycle. However, new research shows that safely retrieving more eggs gives you a greater overall chance of success (2). Your RE will carefully have to balance the number of eggs you can develop to maturity and what is healthy for your body. For example, for some patients, ovarian stimulation medications may put them at risk of ovarian hyperstimulation syndrome (OHSS), a potentially dangerous condition that can develop after egg retrieval, in which the ovaries swell and leak fluid into the abdominal cavity.
After retrieval, the embryologist will check each egg to make sure it is mature, meaning that the egg has shed half of its chromosomes. It’s very common that not all of the eggs retrieved will be mature and ready for fertilization.
Mature Eggs Fertilized with Sperm
After egg retrieval, your eggs will be fertilized with sperm. This can happen by combining eggs and sperm in a petri dish, or through intracytoplasmic sperm injection (ICSI), during which individual sperm are injected directly into each egg. Approximately 70-80% of mature eggs fertilize (3), though this may be different for you.
Embryos Grow to Blastocyst Stage
Over the next 5-7 days, the fertilized eggs will grow into embryos in the lab until they reach the blastocyst stage. At this stage, the embryo has begun to expand and clearly shows a difference in the cells that will form the fetus (inner cell mass, or ICM) and the cells that will form the placenta (trophectoderm, or TE). However, not all the embryos will grow to the blastocyst stage, and not all the blastocyst stage embryos will be of a high enough quality to transfer or freeze.
Less than 50% of embryos are expected to survive to day five, the blastocyst stage, at which time they will be graded by an embryologist to determine which ones are of a high enough quality to transfer and/or freeze.
Receive Genetic Testing Results
At the blastocyst stage of development, you may choose to do preimplantation genetic testing (PGT) on your embryos. This test takes a small number of cells from the TE layer of the embryo (the cells that will form the placenta) and screens them for chromosomal or genetic abnormalities.
A study published in Fertility and Sterility in 2016 found that ~55% of embryos that had reached day 5 of development were chromosomally normal (also known as “euploid”) when maternal age was 27-35. However, the percentage of chromosomally normal embryos steadily decreased with maternal age after 35.
Because of this steady decline in chromosomally normal embryos, older parents concerned about chromosomal abnormalities that may result in miscarriage or lifelong disability for their child may choose to do PGT (6). PGT may also be particularly useful for families worried about genetic disorders and patients experiencing recurrent pregnancy loss (7).

Embryo Transfer
One of the decisions you and your doctor will make before egg retrieval is whether you want to do a fresh or frozen embryo transfer. If you decide to do a fresh transfer, the fertilized eggs will grow in a lab for three to five days before being transferred to the uterus (usually one at a time (8), meaning that one embryo is transferred fresh and the other embryos are frozen for a possible later transfer). With a freeze-all cycle, the fertilized eggs will grow in a lab to the blastocyst stage before being frozen, with the embryo transfer happening at a later date.
There are many instances when embryo transfer does not lead to a live birth. Needing multiple transfers is common (9), especially for older parents, and it’s important to factor that into your plan for IVF.
Pregnancy Confirmation
Getting pregnant is a much anticipated and hoped-for stage of the IVF process. However, with any pregnancy, whether with assisted reproductive technology (ART) or not, there is a risk of miscarriage. Miscarriage is a heartbreaking way to end a pregnancy during the IVF process, even if you are prepared for the possibility.
Below, you can see the percentage of assisted reproductive cycles using fresh embryos from fresh non-donor eggs (meaning that the parent used their own eggs) that resulted in miscarriage, by age (10). It’s important to note that the age of the patient during an IVF cycle is measured when ovarian stimulation begins, not when the embryos are transferred.
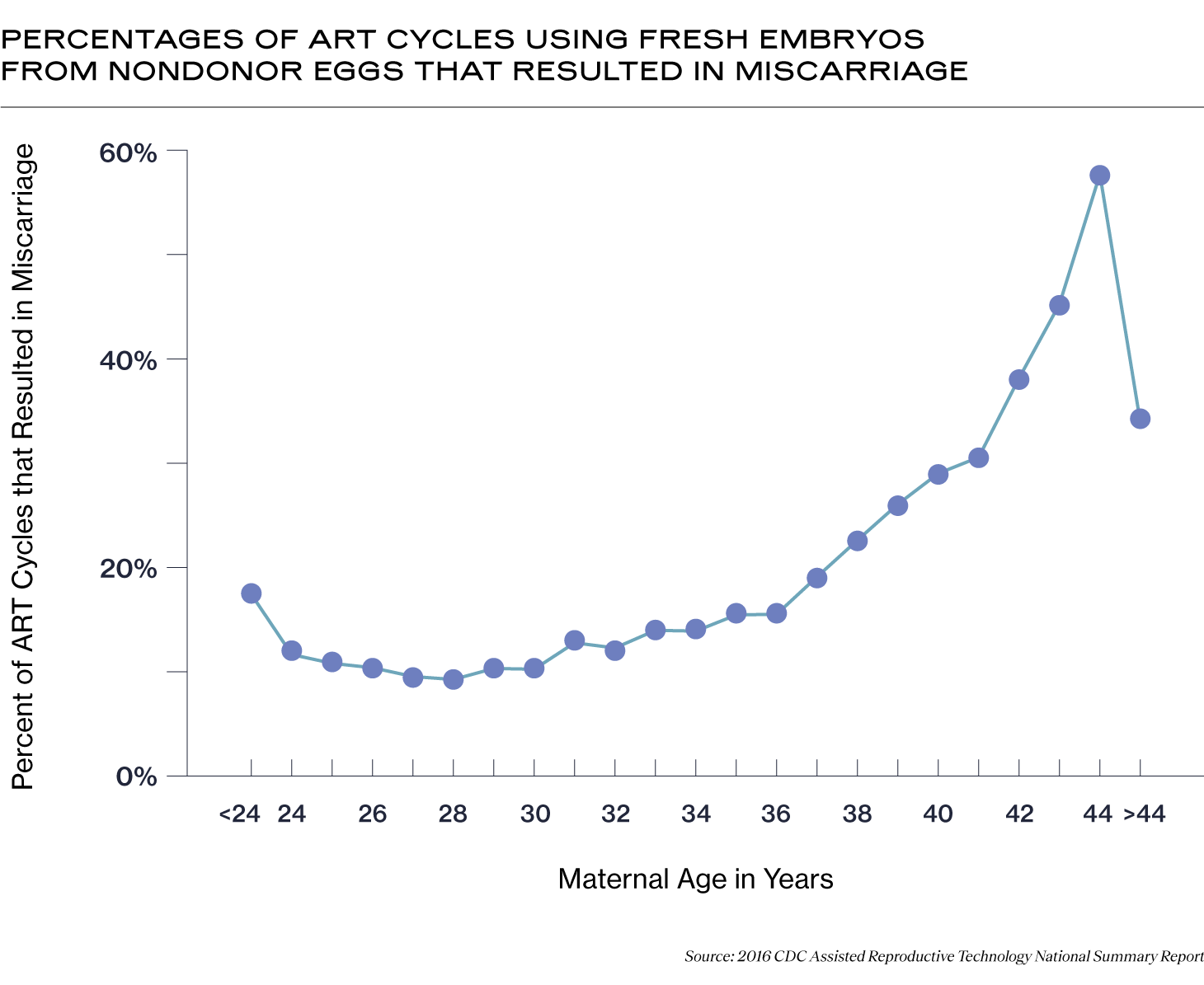
Patients over 42 undergoing IVF may consider PGT for embryos created from their own eggs to decrease the chance of transferring a chromosomally abnormal embryo that may result in miscarriage. Older patients may also consider using donor eggs, for which the IVF miscarriage rates are lower, regardless of the age of the person carrying the baby. According to the 2019 SART National Summary Report, the live birth rate in 2019 using fresh donor eggs was 44.7%, and with frozen donor eggs, it was 40.5% (11).
Undergoing fertility treatment is challenging but not without hope. Knowing about the IVF funnel may help to set expectations for how many cycles you may need to have a baby. There are many factors beyond age that go into success with IVF, and knowing your individual fertility characteristics can also help to set expectations, reduce stress, and sustain hope and energy for the process.
Recent Articles
References
-
Maslow, Bat-Sheva L., et al. “Likelihood of Achieving a 50%, 60%, or 70% Estimated Live Birth Rate Threshold with 1 or 2 Cycles of Planned Oocyte Cryopreservation.” Journal of Assisted Reproduction and Genetics, vol. 37, no. 7, 16 May 2020, pp. 1637–1643, https://doi.org/10.1007/s10815-020-01791-w. Accessed 2 Mar. 2022.
-
Fanton, Michael, et al. “A Higher Number of Oocytes Retrieved Is Associated with an Increase in 2PNs, Blastocysts, and Cumulative Live Birth Rates.” Fertility and Sterility, Jan. 2023, https://doi.org/10.1016/j.fertnstert.2023.01.001. Accessed 27 Feb. 2023.
-
Guerrero, C.A., et al. “Fertilization Rate: A Simple Indirect Marker to Predict Clinical Outcome.” Fertility and Sterility, vol. 94, no. 4, Sept. 2010, p. S147, https://doi.org/10.1016/j.fertnstert.2010.07.591. Accessed 26 Feb. 2023.
-
Speyer, Barbara, et al. “In Assisted Reproduction by IVF or ICSI, the Rate at Which Embryos Develop to the Blastocyst Stage Is Influenced by the Fertilization Method Used: A Split IVF/ICSI Study.” Journal of Assisted Reproduction and Genetics, 9 Jan. 2019, https://doi.org/10.1007/s10815-018-1358-3.
-
Demko, Zachary P., et al. “Effects of Maternal Age on Euploidy Rates in a Large Cohort of Embryos Analyzed with 24-Chromosome Single-Nucleotide Polymorphism–Based Preimplantation Genetic Screening.” Fertility and Sterility, vol. 105, no. 5, May 2016, pp. 1307–1313, www.sciencedirect.com/science/article/pii/S0015028216000662, https://doi.org/10.1016/j.fertnstert.2016.01.025.
-
Munné, Santiago, et al. “Preimplantation Genetic Diagnosis Significantly Reduces Pregnancy Loss in Infertile Couples: A Multicenter Study.” Fertility and Sterility, vol. 85, no. 2, 1 Feb. 2006, pp. 326–332, www.fertstert.org/article/S0015-0282(05)03855-0/fulltext#tbl2, https://doi.org/10.1016/j.fertnstert.2005.10.014. Accessed 12 July 2020.
-
Kim, Julia G., et al. “Preimplantation Genetic Testing for Aneuploidy (PGT-A) Reduces Miscarriage and Improves Live Birth Rates in Recurrent Pregnancy Loss Patients.” Fertility and Sterility, vol. 112, no. 3, Sept. 2019, p. e401, https://doi.org/10.1016/j.fertnstert.2019.07.1141.
-
Mejia, Rachel B., et al. “Elective Transfer of One Embryo Is Associated with a Higher Cumulative Live Birth Rate and Improved Perinatal Outcomes Compared to the Transfer of Two Embryos with in Vitro Fertilization.” F&S Reports, vol. 2, no. 1, 1 Mar. 2021, pp. 50–57, www.fertstertreports.org/article/S2666-3341(20)30098-2/fulltext, https://doi.org/10.1016/j.xfre.2020.10.011. Accessed 28 Feb. 2023.
-
Smith, Andrew D. A. C., et al. “Live-Birth Rate Associated with Repeat in Vitro Fertilization Treatment Cycles.” JAMA, vol. 314, no. 24, 22 Dec. 2015, p. 2654, https://doi.org/10.1001/jama.2015.17296.
-
Centers for Disease Control and Prevention, American Society for Reproductive Medicine, Society for Assisted Reproductive Technology. 2016 Assisted Reproductive Technology National Summary Report. Atlanta (GA): US Dept of Health and Human Services; 2018
-
Society for Assisted Reproductive Technology. Final National Summary Report for 2019. Birmingham, (AL); 2019, https://www.sartcorsonline.com/CSR/PublicSnapshotReport?ClinicPKID=&reportingYear=2019.
Share this
Recent Articles
Learn everything you need to know about IVF
Join the newsletter for IVF education, updates on new research, and early access to Alife products.