IVF Ovarian Stimulation Protocols

Medically reviewed by Linda Streety, RN, BSN
What is an ovarian stimulation protocol?
An in vitro fertilization (IVF) cycle typically starts with the ovarian stimulation process, in which injectable hormone medications are used to stimulate the ovaries to develop multiple mature eggs during your menstrual cycle.
This series, or “protocol,” of medications include:
- medications that stimulate the ovaries to produce multiple eggs
- medications that prevent the ovaries from ovulating those eggs as they develop
- a final trigger shot of hormones that “trigger” the developed eggs to mature together so they can be retrieved during an egg retrieval procedure.
Before selecting your protocol, your reproductive endocrinologist (RE) will order a fertility workup during your last menstrual cycle before ovarian stimulation. This will include blood tests to look at your levels of follicle-stimulating hormone (FSH), luteinizing hormone (LH), estradiol (E2), and anti-müllerian hormone (AMH). (To help you remember all of this new terminology, check out our cheat sheet of the top 12 IVF terms you need to know.) Your results will provide insight into your ovarian reserve (the remaining supply of eggs in your ovaries). Depending on your baseline fertility tests and any infertility diagnoses, your RE will select a protocol of medications designed to help you develop as many eggs as is safe for your body.
Your results will also help your RE understand if you are at risk of developing ovarian hyperstimulation syndrome (OHSS), an uncomfortable and potentially dangerous condition which develops when the ovaries over-respond to the hormone medications used during IVF. Mild cases involve bloating, constipation, reduced urinary output, and abdominal pain. More severe symptoms include rapid weight gain (more than 2.2 pounds in one day), nausea and/or vomiting, severe abdominal pain, and/or shortness of breath. If your RE suspects you are a risk of OHSS, they will select a protocol that minimizes that risk.
What are the most common IVF ovarian stimulation protocols?
Your RE will likely choose one of the commonly used protocols below. The charts should give you a general estimate of how long each protocol will take.
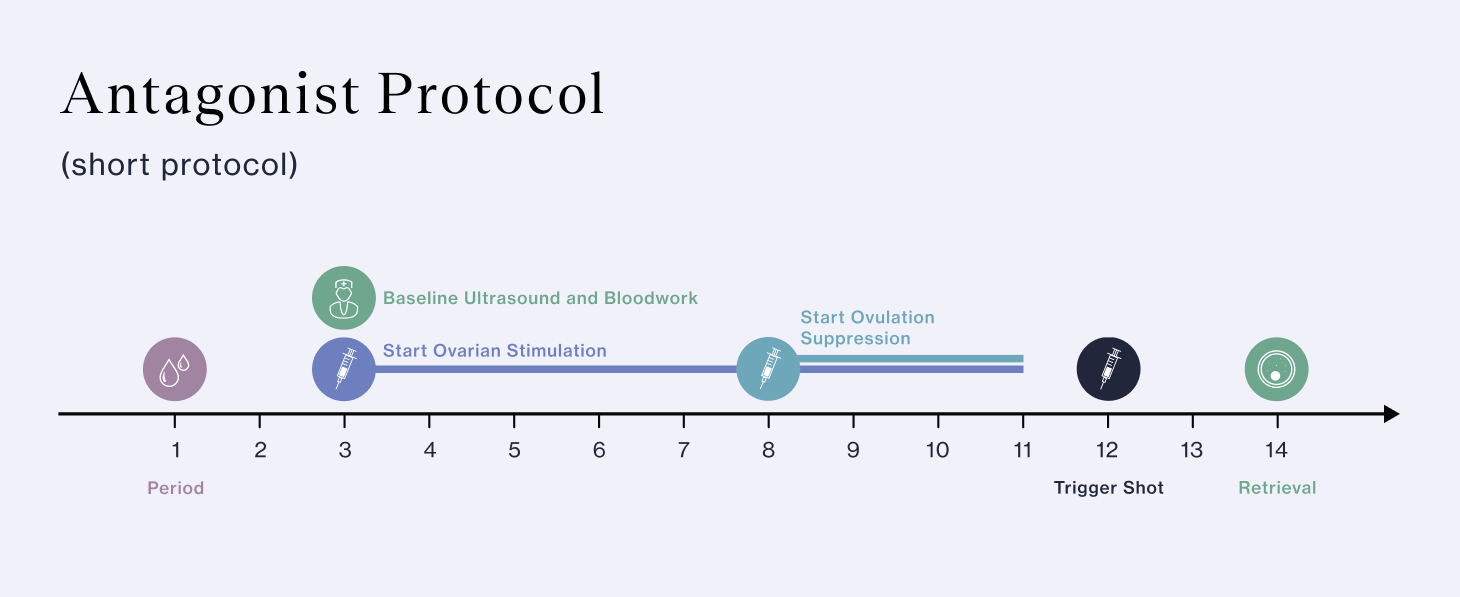
Antagonist protocol (short protocol)
This protocol is now the most commonly used because it uses fewer injectable medications and lasts about 8-14 days. While you can start this protocol with your menstrual cycle, you may also take birth control pills beforehand to control the timing of your IVF cycle. This protocol is suitable for patients at risk of ovarian hyperstimulation syndrome (OHSS). It involves:
- Ovarian stimulation - gonadotropins such as Follistim, Gonal-F, Menopur, or low-dose hCG
- Ovulation suppression - Ganirelix or Cetrotide
- Trigger shot - Lupron, hCG, or a “dual trigger” of Lupron and hCG
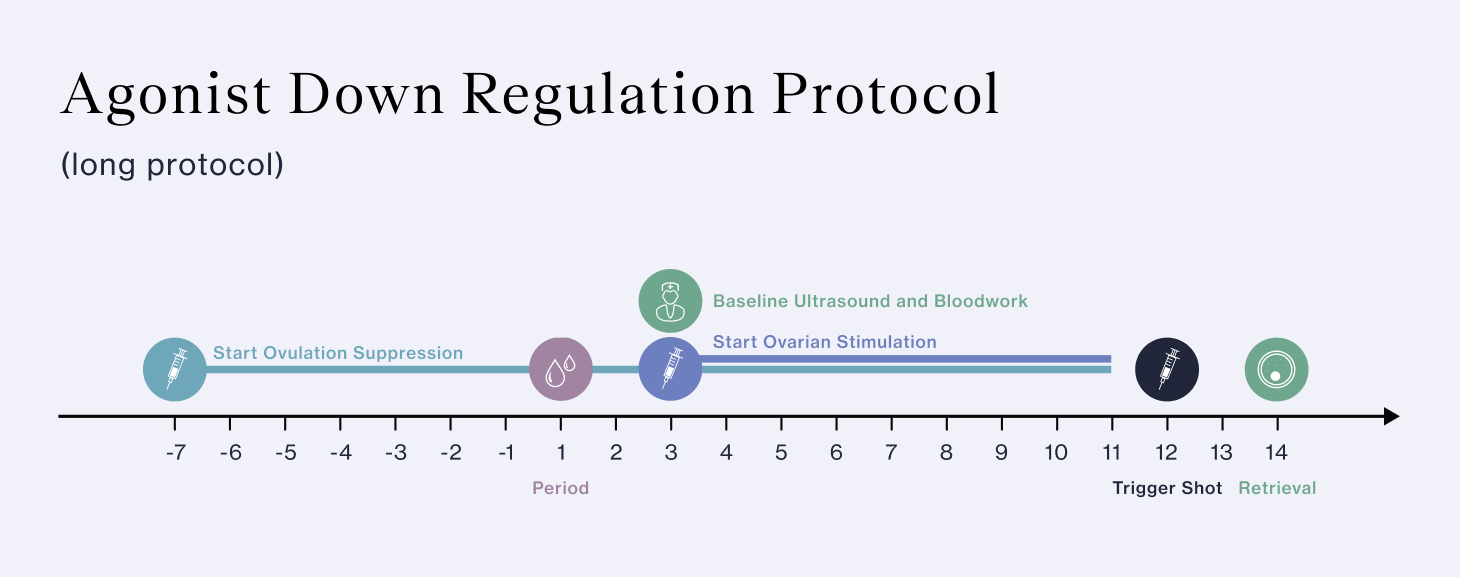
Agonist down regulation protocol (long protocol)
If your RE is concerned about premature ovulation, they may choose this protocol. This protocol is very effective at preventing premature ovulation by using medications to suppress your ovaries before beginning ovarian stimulation. To start this protocol, you may start taking ovulation suppression medications a week before your period, but you may also start ovulation suppression medications on day 1 or 2 of the menstrual cycle before beginning ovarian stimulation. Since this protocol can take as many as 4-5 weeks, it requires more medications. This protocol involves:
- Ovulation suppression - Lupron
- Ovarian stimulation - Follistim, Gonal-F, or Menopur
- Trigger shot - HCG
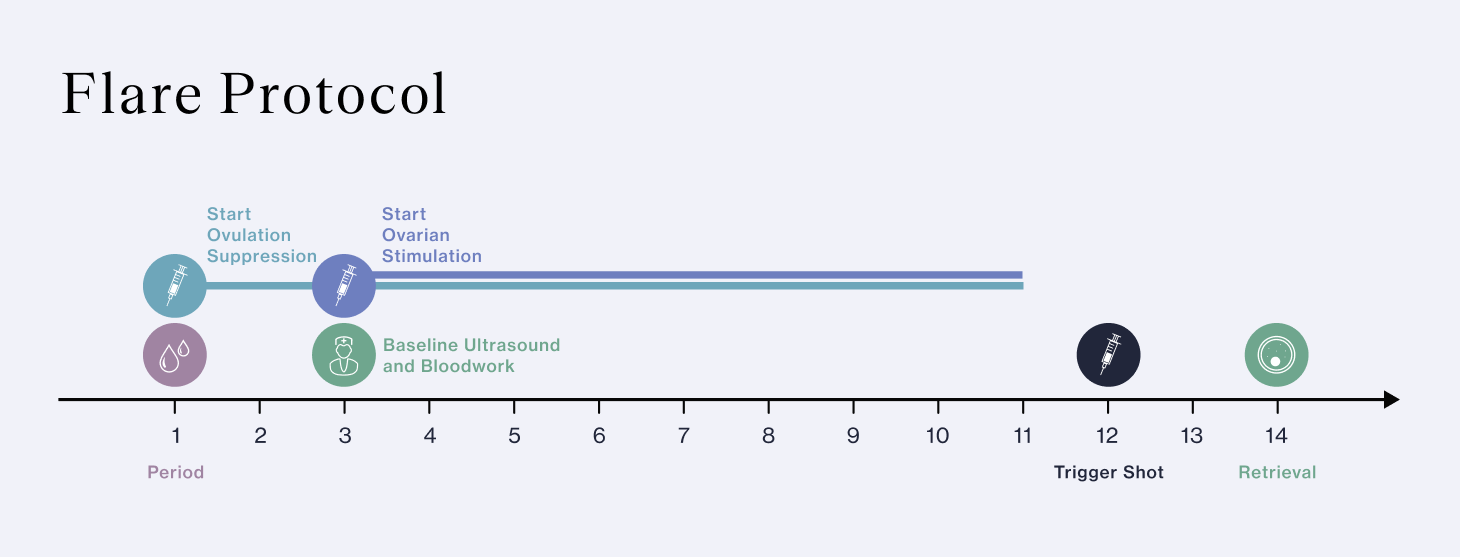
Flare protocol
The flare protocol is a good choice for patients who have responded poorly to other protocols, or who are of advanced maternal age. The flare protocol encourages, rather than suppresses, production of FSH. This protocol involves:
- Ovarian stimulation - Follistim, Gonal-F, or Menopur
- Ovulation suppression - Lupron
- Trigger shot - HCG
While these are the most commonly used protocols, depending on your body and goals, your RE may instead select one of the alternative protocols below.
Mini-IVF
Minimal stimulation IVF or “mini-IVF” may be used if you have low ovarian reserve. Mini-IVF uses lower doses of stimulation medications and may involve oral instead of, or together with, injectable medications. Though mini-IVF is easier on your body, it usually results in just 3-6 eggs retrieved, lowering your chance of success.
Stop Lupron Protocol
Your RE may choose this protocol if you are a low responder, which typically means you are an older patient with low ovarian reserve. Stop Lupron is similar to the agonist down regulation protocol but uses lower doses of Lupron, and stops Lupron administration after your period and before starting ovarian stimulation medications.
Progestin-Primed Stimulation
During your usual menstrual cycle, the pituitary gland releases luteinizing hormone (LH) to trigger your egg (or eggs) to mature. This relatively new protocol uses progestin to suppress that LH surge. So far, studies have shown that this medication protocol has similar success rates as other protocols (1). The advantage is that it involves more oral medications and fewer shots (2). The disadvantage is that you may not be able to do a fresh embryo transfer and need to freeze your embryos.
Estrogen Priming Protocol
This protocol is very similar to the antagonist (short) protocol, only it includes estrogen supplementation in the form of patches, pills, or injections. Your RE may select this protocol if you have low ovarian reserve, because it’s believed to help increase the number of follicles available for stimulation and help them grow at the same time.
Natural Cycle IVF
This type of IVF doesn’t involve any stimulation medications. Instead, your clinician will carefully monitor your usual menstrual cycle and retrieve the egg once it has matured, but before ovulation. Because timing is so critical and you will usually only retrieve one egg, the success rate of IVF with a natural cycle is considerably lower than with stimulation medications. However, for patients who are unable to take stimulation medications, it is an important option.
Should I try a different protocol if my first IVF cycle wasn’t successful?
Many patients need more than one IVF cycle to have a baby. If that’s the case for you, your RE will use your results from your first cycle (or cycles) to tailor your medications for your next cycle and optimize the number of eggs they can retrieve. They may even change your protocol. This is important because new research shows that your overall chance of success will be better if you retrieve as many as is safely possible for your body. Each egg retrieved increases your chance of success with IVF, since each egg increases the possibility of a high quality embryo for transfer.
It may be helpful to know that if your first cycle was not successful, that doesn’t mean that you have a worse chance of success with your next cycle. In fact, data shows that even when patients use the exact same medication protocol, they tend to retrieve more eggs and develop more blastocysts with subsequent cycles.
It’s important to note that the number of eggs your RE retrieves will most likely not be the same as the number of embryos you will have from your IVF cycle. This is because some eggs and embryos don’t make it to the next step of the IVF process. To help understand why this happens and to get a sense of how many eggs and embryos are average for your age, it may help to understand the "IVF funnel."
Do higher doses of medications = more eggs?
The goal of ovarian stimulation is to safely maximize the number of eggs that your body can produce. Each patient has a maximum number of follicles that develop with each menstrual cycle. Your RE will aim for a protocol that aims to develop most of those follicles to maturity. Because this process requires managing a delicate series of hormones, more medications don’t necessarily correspond with more eggs. Instead, your RE will aim to give you the optimal dose of each medication at the optimal time. This gives you the best chance of success.
While very rare, severe OHSS can be a serious complication of ovarian stimulation. If you are at risk of OHSS, current protocols can help you retrieve the optimum number of eggs while minimizing your risk of OHSS.
Recent Articles
References
-
Yildiz, S., Turkgeldi, E., & Ata, B. (2023). Role and effectiveness of progestins in pituitary suppression during ovarian stimulation for assisted reproductive technology: a systematic review and a meta-analysis. Minerva Obstetrics and Gynecology, 75(6), 573–582. https://doi.org/10.23736/S2724-606X.22.05176-4
-
Ata, B., & Erkan Kalafat. (2023). Progestin primed ovarian stimulation, for whom, when and how? Reproductive Biomedicine Online, 103639–103639. https://doi.org/10.1016/j.rbmo.2023.103639
Share this
Recent Articles
Learn everything you need to know about IVF
Join the newsletter for IVF education, updates on new research, and early access to Alife products.